Key Points
Preeclampsia is a kind of high blood pressure some women get after the 20th week of pregnancy or after giving birth.
Most pregnant women with preeclampsia have healthy babies. But if not treated, it can cause serious problems, like preterm birth and even death.
If you’re at risk for preeclampsia, your provider may want you take low-dose aspirin to help prevent it.
If you have blurred vision, swelling in your hands and face or severe headaches or belly pain, call your provider right away.
You can have preeclampsia and not know it, so go to all of your prenatal care visits, even if you’re feeling fine.
Download our English and Spanish health action sheets on low-dose aspirin.
What is preeclampsia?
Preeclampsia is a serious condition that can happen after the 20th week of pregnancy or after giving birth (called postpartum preeclampsia). In addition to causing high blood pressure, it can cause organs, like the kidneys and liver, to not work normally. Blood pressure is the force of blood that pushes against the walls of your arteries. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. Arteries are blood vessels that carry blood away from your heart to other parts of the body. Having high blood pressure can stress your heart and cause problems during pregnancy.
Preeclampsia is a serious health problem for women around the world. Between 10 to 15 percent of maternal deaths worldwide are caused by preeclampsia and associated complications, such as eclampsia. In the United States, it affects between 5 to 8 percent of pregnancies, and in most cases leads to preterm birth. Preterm birth is birth that happens too early, before 37 weeks of pregnancy.
Most women with preeclampsia have healthy babies. But if not treated, it can cause severe health problems for you and your baby.
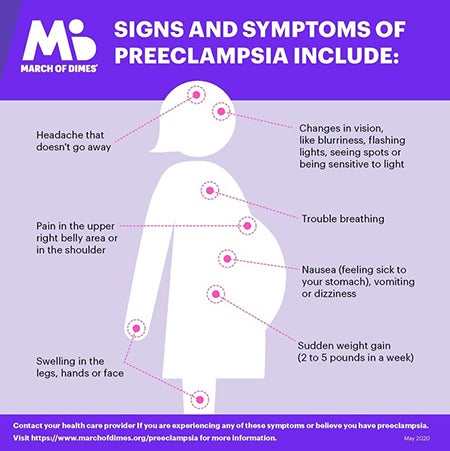
What are the signs and symptoms of preeclampsia?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
Signs and symptoms of preeclampsia include:
- High blood pressure with or without protein in the urine. Your provider will check these during your prenatal visit.
- Changes in vision, like blurriness, flashing lights, seeing spots or being sensitive to light
- Headache that doesn’t go away
- Nausea (feeling sick to your stomach), vomiting or dizziness
- Pain in the upper right belly area or in the shoulder
- Sudden weight gain (2 to 5 pounds in a week)
- Swelling in the legs, hands or face
- Trouble breathing
Many of these signs and symptoms are common discomforts of pregnancy. If you have even one sign or symptom, call your provider right away. Sometimes you don't realize you have preeclampsia. Go to all your prenatal visits, even if you feel fine. That’s the best way to detect preeclampsia.
Can taking low-dose aspirin help reduce your risk for preeclampsia and preterm birth?
For some women, yes. If your provider thinks you’re at risk for preeclampsia, low-dose aspirin may be recommended to help prevent it. Low-dose aspirin also is called baby aspirin or 81 mg (milligrams) aspirin. Talk to your provider to see if treatment with low-dose aspirin is right for you.
You can buy low-dose aspirin over-the-counter, or your provider can give you a prescription for it. If your provider wants you to take low-dose aspirin to help prevent preeclampsia, take it exactly as it’s recommended. Don’t take more or take it more often than your provider says.
If you’re at high risk for preeclampsia, your provider may want you to start taking low-dose aspirin after 12 weeks of pregnancy. If you have diabetes or high blood pressure, your provider may ask you to take low-dose aspirin.
According to the American College of Obstetricians and Gynecologists (also called ACOG), daily low-dose aspirin use in pregnancy has a low risk of serious complications and its use is considered safe.
Are you at risk for preeclampsia?
We don’t know for sure what causes preeclampsia, but there are some things that may make you more likely than other women to have it. These are called risk factors. If you have even one risk factor for preeclampsia, tell your provider.
You’re at high risk for preeclampsia If:
- You’ve had preeclampsia in a previous pregnancy. The earlier in pregnancy you had preeclampsia, the higher your risk is to have it again. You’re also at higher risk if you had preeclampsia along with other pregnancy complications.
- You’re pregnant with multiples (twins, triplets or more).
- You have high blood pressure, diabetes, kidney disease or an autoimmune disease like lupus or antiphospholipid syndrome. Diabetes is when your body has too much sugar in the blood. This can damage organs, like blood vessels, nerves, eyes and kidneys. An autoimmune disease is a health condition that happens when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake.
Other risk factors for preeclampsia:
- You’ve never had a baby before, or it’s been more than 10 years since you had a baby.
- You’re a person who has obesity. Obese means being very overweight with a body mass index (also called BMI) of 30 or higher. To find out your BMI, go to www.cdc.gov/bmi.
- You have a family history of preeclampsia. This means that other people in your family, like your sister or mother, have had it.
- You had complications in a previous pregnancy, like having a baby with low birthweight. Low birthweight is when your baby is born weighing less than 5 pounds, 8 ounces.
- You had fertility treatment called in vitro fertilization (also called IVF) to help you get pregnant.
- You’re older than 35.
Some groups, such as African-American women and those who are affected by lower income, are also at higher risk of complications like preeclampsia. Historically, in the United States, these groups have had a harder time getting good quality health care and access to treatments that prevent illness. This has led to serious health disparities and unequal health outcomes. Talk to your provider about your risk factors and about what you can do to stay healthy and reduce your chances of having a preterm birth. If your provider thinks you’re at risk of having preeclampsia, ask if treatment with low-dose aspirin is right for you.
How can preeclampsia affect you and your baby?
Without treatment, preeclampsia can cause serious health problems for you and your baby, even death. You may have preeclampsia and not know it, so be sure to go to all your prenatal care checkups, even if you’re feeling fine. If you have any sign or symptom of preeclampsia, tell your provider.
Health problems for women who have preeclampsia include:
- Kidney, liver and brain damage
- Problems with how your blood clots. A blood clot is a mass or clump of blood that forms when blood changes from a liquid to a solid. Your body normally makes blood clots to stop bleeding after a scrape or cut. Problems with blood clots can cause serious bleeding problems.
- Eclampsia. This is a rare and life-threatening condition. It’s when a pregnant woman has seizures or a coma after preeclampsia. A coma is when you’re unconscious for a long period of time and can't respond to voices, sounds or activity.
- Stroke. This is when the blood supply to the brain is interrupted or reduced. Stroke can happen when a blood clot blocks a blood vessel that brings blood to the brain, or when a blood vessel in the brain bursts open.
Pregnancy complications from preeclampsia include:
- Preterm birth. Even with treatment, you may need to give birth early to help prevent serious health problems for you and your baby.
- Placental abruption. This is when the placenta separates from the wall of the uterus (womb) before birth. It can separate partially or completely. If you have placental abruption, your baby may not get enough oxygen and nutrients. Vaginal bleeding is the most common symptom of placental abruption after 20 weeks of pregnancy. If you have vaginal bleeding during pregnancy, tell your health care provider right away.
- Intrauterine growth restriction (also called IUGR). This is when a baby has poor growth in the womb. It can happen when mom has high blood pressure that narrows the blood vessels in the uterus and placenta. The placenta grows in the uterus and supplies your baby with food and oxygen through the umbilical cord. If your baby doesn’t get enough oxygen and nutrients in the womb, he may have IUGR.
- Low birthweight
Having preeclampsia increases your risk for postpartum hemorrhage (also called PPH). PPH is heavy bleeding after giving birth. It’s a rare condition, but if not treated, it can lead to shock and death. Shock is when your body’s organs don’t get enough blood flow.
Having preeclampsia increases your risk for heart disease, diabetes and kidney disease later in life.
How is preeclampsia diagnosed?
To diagnose preeclampsia, your provider measures your blood pressure and tests your urine for protein at every prenatal visit. Additional lab work evaluating your blood count, clotting factors, liver and kidney function are also assessed.
Your provider may check your baby’s health with:
- Ultrasound. This is a prenatal test that uses sound waves and a computer screen to make a picture of your baby in the womb. Ultrasound checks that your baby is growing at a normal rate. It also lets your provider look at the placenta and the amount of fluid around your baby to make sure your pregnancy is healthy.
- Nonstress test. This test checks your baby’s heart rate.
- Biophysical profile. This test combines the nonstress test with an ultrasound.
- Doppler analysis. This is a sonographic test to evaluate the blood flow through the baby’s umbilical cord -- it can provide information as to how blood flow -- which carries oxygen - is getting to your baby
Treatment depends on how severe your preeclampsia is and how far along you are in your pregnancy. Even if you have mild preeclampsia, you need treatment to make sure it doesn’t get worse.
How is mild preeclampsia treated?
Most women with mild preeclampsia are delivered by 37 weeks of pregnancy . If you have mild preeclampsia before 37 weeks:
- Your provider checks your blood pressure and urine regularly. It’s possible that you may need to stay in the hospital to be monitored closely. If you’re not in the hospital, your provider may want you to have checkups once or twice a week. You may also need to take your blood pressure at home.
- Your provider may ask you to do kick counts to track how often your baby moves. There are two ways to do kick counts: Every day, time how long it takes for your baby to move ten times. If it takes longer than 2 hours, tell your provider. Or three times a week, track the number of times your baby moves in 1 hour. If the number changes, tell your provider.
- If you’re at least 37 weeks pregnant and your condition is stable, your provider may recommend that you have your baby early. This may be safer for you and your baby than staying pregnant. Your provider may give you medicine or break your water (amniotic sac) to make labor start. This is called inducing labor.
How is severe preeclampsia treated?
If you have severe preeclampsia, you most likely stay in the hospital so your provider can closely monitor you and your baby. Your provider may treat you with medicines called antenatal corticosteroids (also called ACS). These medicines help speed up your baby’s lung development. You also may get medicine to control your blood pressure and medicine to prevent seizures (called magnesium sulfate).
If your condition gets worse, it may be safer for you and your baby to give birth early. Most babies of moms with severe preeclampsia before 34 weeks of pregnancy do better in the hospital than by staying in the womb. If you’re at least 34 weeks pregnant, your provider may recommend that you have your baby as soon as your condition is stable. Your provider may induce your labor, or you may have a c-section. If you’re not yet 34 weeks pregnant but you and your baby are stable, you may be able to wait to have your baby.
If you have severe preeclampsia and HELLP syndrome, you almost always need to give birth early. HELLP syndrome is a rare but life-threatening liver disorder. About 2 in 10 women (20 percent) with severe preeclampsia develop HELLP syndrome. You may need medicine to control your blood pressure and prevent seizures. Some women may need blood transfusions. A blood transfusion means you have new blood put into your body.
If you have preeclampsia, can you have a vaginal birth?
Yes. If you have preeclampsia, a vaginal birth may be better than a cesarean birth (also called c-section). A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. With vaginal birth, there's no stress from surgery. For most women with preeclampsia, it’s safe to have an epidural to manage labor pain as long as your blood clots normally. An epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief during labor.
What is postpartum preeclampsia?
Postpartum preeclampsia is a rare condition. It’s when you have preeclampsia after you’ve given birth. It most often happens within 48 hours (2 days) of having a baby, but it can develop up to 6 weeks after a baby’s birth. It’s just as dangerous as preeclampsia during pregnancy and needs immediate treatment. If not treated, it can cause life-threatening problems, including death.
Signs and symptoms of postpartum preeclampsia are like those of preeclampsia. It can be hard for you to know if you have signs and symptoms after pregnancy because you’re focused on caring for your baby. If you do have signs or symptoms, tell your provider right away.
We don’t know exactly what causes postpartum preeclampsia, but these may be possible risk factors:
- You had gestational hypertension or preeclampsia during pregnancy. Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth.
- You’re obese.
- You had a c-section.
Complications from postpartum preeclampsia include these life-threatening conditions:
- HELLP syndrome
- Postpartum eclampsia (seizures). This can cause permanent damage to our brain, liver and kidneys. It also can cause coma.
- Pulmonary edema. This is when fluid fills the lungs.
- Stroke
- Thromboembolism. This is when a blood clot travels from another part of the body and blocks a blood vessel.
Your provider uses blood and urine tests to diagnose postpartum preeclampsia. Treatment can include magnesium sulfate to prevent seizures and medicine to help lower your blood pressure. Medicine to prevent seizures also is called anticonvulsive medicine. If you’re breastfeeding, talk to your provider to make sure these medicines are safe for your baby.
Reviewed January 2023